Tricuspid Atresia
What is Tricuspid Atresia?
- (© Competence Network for Congenital Heart Defects)
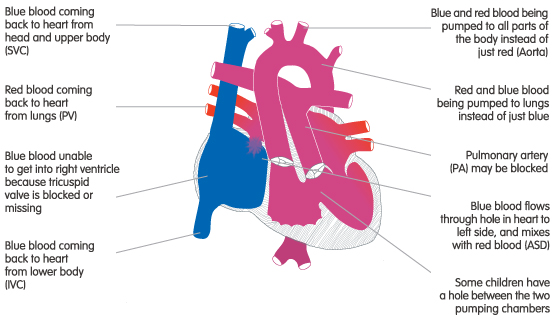
Tricuspid refers to the tricuspid valve. Atresia means closed or absent.
So Tricuspid Atresia means:
- The tricuspid valve is closed or absent;
- The right ventricle is smaller than in a normal heart;
- The pulmonary artery is narrower than in a normal heart; and
- The pulmonary valve may be blocked.
The tricuspid valve is the gateway between the right atrium and the right ventricle. Therefore, when it is closed or missing blue (deoxygenated) blood cannot be pumped through the right side of the heart to the lungs.
Babies born with Tricuspid Atresia will only survive if they have either:
- A hole between the atria – an atrial septal defect (ASD), and a hole between the ventricles – a ventricular septal defect (VSD). The ASD allows blood to cross from the right atrium into the left atrium. From there it can go through the mitral valve and into the left ventricle. Most of it will then be pumped into the aorta, but some will cross through the VSD into the right ventricle. This blood is then pumped into the pulmonary artery (if it is not blocked) which takes it to the lungs; or
- A ductus arteriosus - this is a part of our circulation before we are born. It links the aorta to the pulmonary artery, thus allowing some blood to get to the lungs. Normally the ductus will close shortly after birth, but for a baby with tricuspid atresia this can be fatal. Therefore, doctors will try to keep the ductus arteriosus open until surgery can be performed.
Diagnosis
Your baby may have been diagnosed with Tricuspid Atresia before birth during a scan of the foetal heart.
If the heart condition was not detected before birth, your baby will probably start to show symptoms soon after they are born. Doctors will then be able to diagnose the condition.
Babies born with Tricuspid Atresia do not have enough blue (deoxygenated) blood travelling from their heart to their lungs. This in turn, means that there is not enough red (oxygenated blood) travelling from the lungs back to the heart and on to the rest of the body. If there is not enough oxygenated (red) blood being pumped around the body then your baby may look blue (cyanosis) and be breathless. This breathlessness can make it difficult for them to feed properly.
Doctors may also detect a heart murmur - the sound of the blood moving in the wrong direction through the heart. If the pulmonary artery is narrowed (stenotic) these symptoms will be apparent very soon after birth.
Doctors can use the following tests to help them make their diagnosis:
- Pulse, blood pressure, temperature, and number of breaths a baby takes a minute;
- Listening with a stethoscope for changes in the heart sounds;
- An oxygen saturation monitor to see how much oxygen is getting into the blood;
- A chest x-ray to see the size and position of the heart;
- An ECG (electrocardiogram) to check the electrical activity;
- An ultrasound scan (echocardiogram) to see how the blood moves through the heart;
- Checks for chemical balance in blood and urine; and
- A catheter or Magnetic resonance Imaging (MRI) test.
Treatment
The treatment for tricuspid atresia is palliative. This means that your child’s heart cannot be made to work like a normal heart, but it can be made to work better (palliated).
Medicine
Your child will need medicine to keep the ductus arteriosus open, and hence improve the blood flow to the lungs, as soon as they are born.
BT Shunt
Your child may need a shunt (connection) to increase the amount of blood getting to the lungs. This is done soon after birth by connecting a tube from an artery in the arm to the pulmonary arteries. This operation may be carried out through the side of the chest, while the heart is beating, or through the front using a heart lung bypass machine (open heart surgery).
Surgery
Your child will need further surgery to improve the amount of blue blood travelling to the lungs to get oxygen. Depending on your child’s condition, this may be:
- A Glenn / Bi-directional Glenn - this involves making a passage between the superior vena cava (the big vein bringing blue blood from the upper body to the heart) to the right pulmonary artery. This will let a much larger amount of blue blood flow into the lungs where it can get oxygen; or
- A Fontan procedure - this operation joins the inferior vena cava (vein bringing blue blood from the lower body to the heart) to the pulmonary arteries. This means that all blood returning to the heart from the body is forced to pass through the lungs where it can get oxygen.
Both of these operations involve open heart surgery, which means that the heart will need to be stopped and opened to repair it. During the operation, a machine called the heart bypass machine will take over the job that the heart and lungs normally do.
How your child is affected
It may take some time for your child to recover from open heart surgery. They will probably spend time in an intensive care or high dependency unit, while the heart and lungs adjust to the different pressures. After that they will be moved to a cardiac ward where they may still need to spend up to several weeks.
Scars on the chest fade very rapidly after surgery in most children, but they will not go altogether. Smaller scars on the hands and neck usually fade away to nothing.
Some children will need to continue on diuretic medicines to help them get rid of excess fluid. In some cases an anticoagulant (anti-clotting) medicine, such as aspirin or warfarin, will be prescribed. This is because the child’s blood will be flowing at low pressure (because their right ventricle is not able to pump blood) and this could cause a blood clot. If your child is on warfarin, the level of anticoagulation has to be monitored frequently using a blood test.
Your child may develop more slowly at first than other children of the same age. They may also tire quickly, due to the lack of oxygen in their bloodstream. However, if the palliative surgery is successful, then they should be able to catch up with others of the same age, and take part in normal activities.
Some of these problems can occur after surgery or later in life:
- It is common for the valves to leak a little. If this becomes severe, they may need to be repaired or even replaced with an artificial valve. If the valve is replaced, the new valve will need to be monitored to make sure it works effectively. Artificial valves may also need to be replaced as the child grows. Children with artificial valves need to take anticoagulants for the rest of their lives, which can have a number of implications for their health and lifestyle.
- Your child may develop a very fast heart beat (tachycardia). This may need to be treated with medicines – antiarrhythmic drugs.


